AVN Patient Information
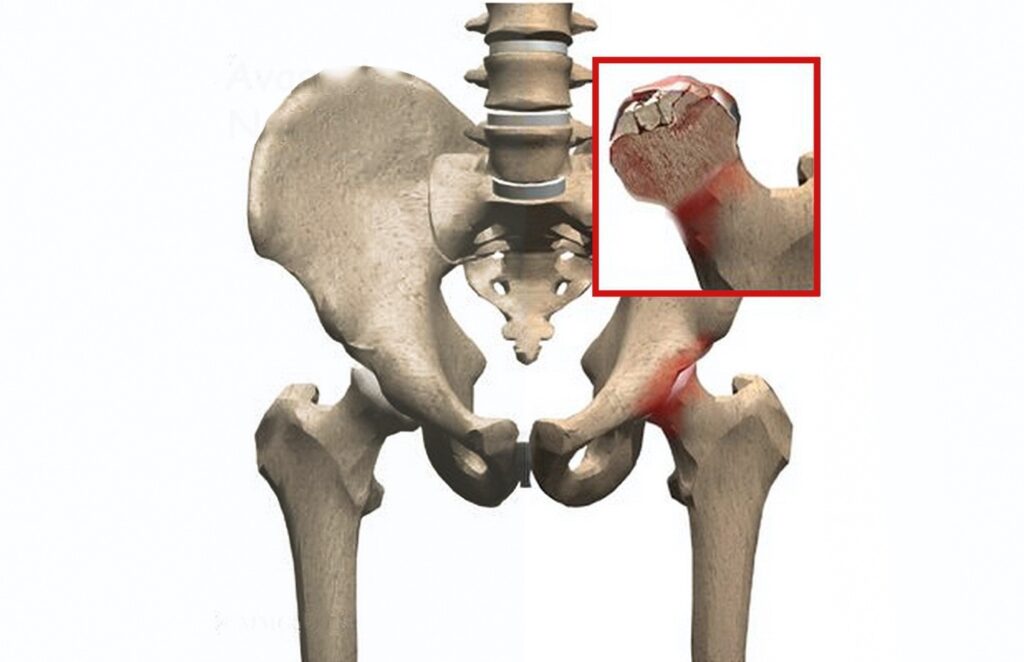
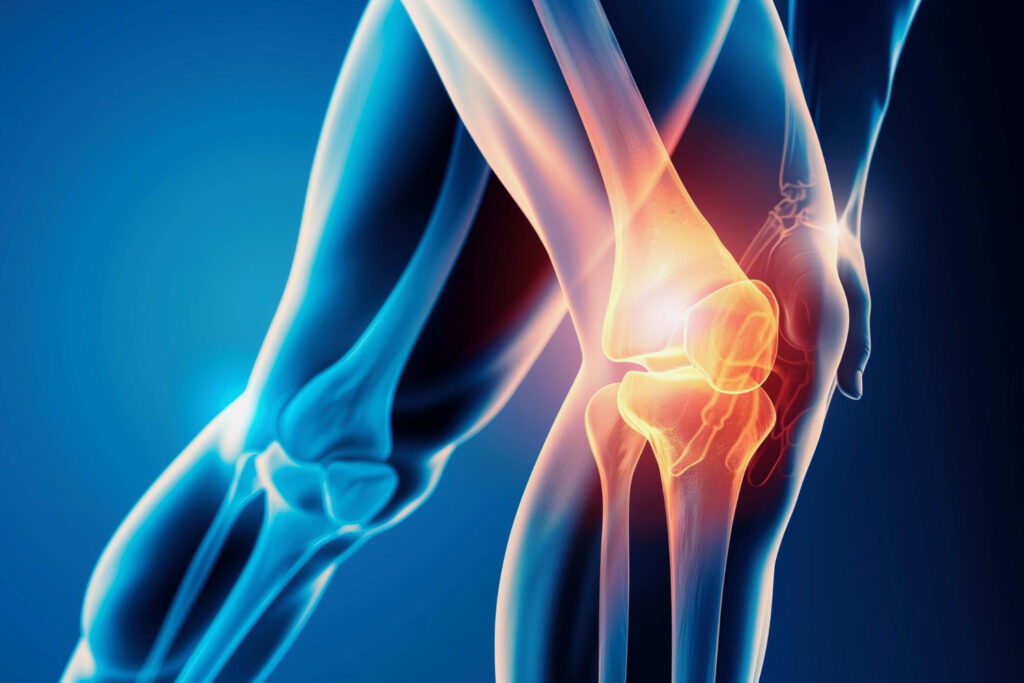
“AVN (Avascular OsteoNecrosis) Is a condition where the blood supply to the bone is blocked. This leads to death and necrosis with pain and eventual collapse of the affected bone, most commonly seen in the hip (femoral head) with crippling pain. The incidence of AVN has increased recently after COVID-19 Pandemic. This, if identified early, can be treated medically.” UNDERSTANDING THE DISEASE OF AVASCULAR NECROSIS Avascular Necrosis (AVN) or Osteonecrosis of the femoral head is a pathological process that results from interruption of blood supply to the bone which leads to the death of marrow and osteocytes resulting in collapse of the necrotic segment of the femoral head. In the early stages of the disease, there is severe pain from the dying bone. Later this leads to frank arthritis of the hip, causing stiffness, limitation of movement and adds to the disability of the patient in day to day routine life. This is the most common cause of total hip replacement in young patients in India. ETIOLOGY : Avascular Necrosis (AVN) is often seen in association with a number of different conditions. Trauma with fracture of the femoral neck, especially in the sub-capital region, interrupts the major part of the blood supply to the head and may lead to AVN. The risk has been reported to be as high as 10% -40% after a displaced femoral neck fracture. Some of the factors leading to AVN are : PATHOGENESIS : The hematopoietic cells are most sensitive to Anoxia (due to interruption of blood supply causing inadequate oxygenation). Ischaemia causes death of marrow cells, death of bone cells causing necrosis of the affected segment which leads to weakness and collapse of the femoral head. This in turn causes incongruity leading to arthritis of the hip joint. Nature tries to heal this condition through removal of dead cells by osteoclasts and layering of new bone cells by osteoblasts. This natural process of healing takes upto three years, the life cycle of the disease. There are four stages (Ficat & Arlet) of AVN of the femoral head based on the clinical and radiological presentation. Stage 1 the normal congruity of the femoral head is maintained with minimal symptoms and Stage IV is the end stage with collapse of the hip with arthritis. SYMPTOMS : Patients with AVN have a varied presentation based on their involvement of the femoral head (Stage of AVN). In early stages, patients present with groin, buttock, thigh pain or even with the knee pain with normal x-rays and an abnormal MRI. In later stages, patient present there is a limp, limitation or decreased movements of the hip joint and restriction of activities of daily living. INVESTIGATIONS : Standard plain x-rays of pelvis with both hips (PBH view) and MRI helps in making a diagnosis as well as prognosis of the conditions. In certain cases, radio-nuclide bone scan also helps. Standard plain x-rays of pelvis with both hips (PBH view) and MRI helps in making a diagnosis as well as prognosis of the conditions. METHODS OF TREATMENT : SURGICAL MANAGEMENT There are various surgical procedures which have been described such as core decompression, vascular fibular bone grafting, osteotomies around the femoral head and vascular pedicle graft, with varied success rate. All these surgical procedures help in early stages of AVN with variable success but adds morbidity to patient. Stem cells implantation is still in experimental stage. The only consistent good results are seen in total joint replacements. MEDICAL MANAGEMENT INVOLVES : It is combined with Calcium, Vit B12, Folic acid supplements. Bisphosphonate therapy, the only currently available peer reviewed and proven in world literature.